Abstract
Introduction. The presence and severity of heart involvement at diagnosis is by far the most important prognostic factor in AL amyloidosis, and our ability to prognosticate survival and assess response to therapy based on cardiac biomarkers has revolutionized the management of this disease. However, very little is known on the impact of persisting cardiac dysfunction after upfront chemotherapy in patients with AL amyloidosis. This is particularly relevant to identify subjects who can benefit most from the different therapies targeting amyloid deposits that are currently being tested in clinical trials in patients who still have cardiac dysfunction after successful upfront therapy.
Methods. The prospectively maintained database of the Pavia Amyloidosis Research and Treatment Center was searched for patients who obtained at least a partial hematologic response (PR) after upfront therapy. Survival was measured from the time of best hematologic response to death or last follow-up. Cutoffs of N terminal pro natriuretic peptide type B (NT-proBNP) best predicting survival after response were identified by Receiver Operator Characteristic (ROC) analyses based on death at 2 years.
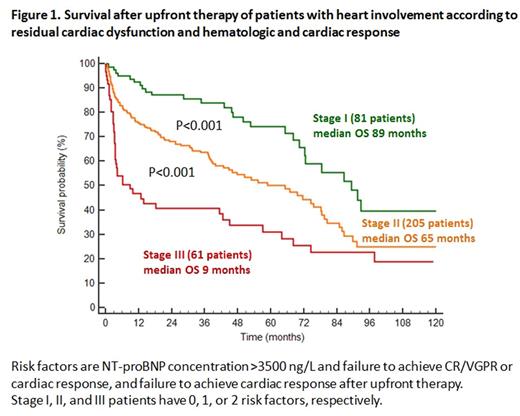
Results. A total of 507 patients diagnosed between 2004 and 2015 were included in the study. Best hematologic response was achieved after a median of 3.6 months from upfront therapy initiation and was complete response (CR) in 22%, very good PR (VGPR) in 56%, and PR in 22%. At diagnosis the heart was involved in 77% of patients. After a median follow-up of living patients of 52 months, median overall survival (OS) from the time of best response was 76 months. Median OS by response category was not reached for CR, 78 months for VGPR (P=0.004 compared to CR), and 40 months for PR (P<0.001 compared to VGPR). The presence of heart involvement remained a predictor of poorer survival also after achievement of hematologic response (median 70 months vs. not reached, P<0.001). Baseline NT-proBNP was >650 ng/L (evaluable for cardiac response) in 347 patients (68%). Of them, 121 [35%, 95% confidence interval (CI) 29-42%] achieved a cardiac response by the time of best hematologic response. Cardiac response was associated with improved survival (median 86 vs. 46 months, P<0.001). The cutoff of NT-proBNP concentration best predicting survival after hematologic response was 3500 ng/L (median 16 vs. 93 months, P<0.001). Importantly, patients whose NT-proBNP was <3500 ng/L had a longer survival within each hematologic response category (CR median not reached vs. 74 months, P=0.012; VGPR median not reached vs. 21 months, P<0.001; PR median 50 vs. 4 months, P<0.001). At multivariate analysis achievement of CR/VGPR after upfront therapy [hazard ratio (HR) 0.54, 95%CI 0.39-0.75, P<0.001], a concentration of NT-proBNP above 3500 ng/L (HR 2.61, 95%CI 1.88-3.63, P<0.001), and NT-proBNP response (HR 0.68, 95%CI 0.48-0.98, P=0.036) were independent predictors of survival. The quality of response (achievement of CR/VGPR and/or cardiac response) and NT-proBNP concentration (cutoff 3500 ng/L) identified 3 groups with significantly different survivals after upfront therapy (Figure 1).
Discussion. In AL amyloidosis heart dysfunction persisting after achievement of best hematologic response retains its ominous prognostic impact also in patients obtaining good quality hematologic response. A novel staging system incorporating NT-proBNP concentration and hematologic and cardiac response allows best prediction of survival of patients with heart involvement after response to upfront therapy, identifying those in greater need of further improving heart involvement and/or quality of hematologic response.
Palladini: Prothena: Honoraria, Other: Travel grant; Celgene: Other: Travel grants; Jannsen-Cilag: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal